The year 2025 has brought sharp contrasts in digital health. On one side there is a surge in adoption with nearly 19% of U.S. primary care visits now conducted virtually. On the other side patients continue to report high levels of frustration. A global survey shows 86% of people would pay more for better service. In medicine dissatisfaction does not simply hurt a brand. It affects adherence outcomes and trust.

Why Pain Points Matter
Pain points in digital health are not minor details. They are the barriers that determine whether patients continue to use a service, whether clinicians adopt a platform, and whether outcomes improve. Every step of the digital journey can contain obstacles. A confusing registration page, an unclear insurance form, or a delayed follow-up message may appear small, yet together they shape trust. When friction builds up, patients often disengage, which reduces adherence to treatment and increases system costs. Evidence shows that people who encounter negative digital experiences are about 10% more likely to avoid preventive care. That small percentage translates into thousands of missed screenings, later diagnosis of chronic disease, and avoidable hospitalizations that place additional pressure on health systems.
Patient experience is not only about satisfaction surveys. In medicine it influences measurable health outcomes. If patients cannot easily access digital appointments or find information on medication, the result is not just frustration. It may mean untreated hypertension, unmanaged diabetes, or undetected cancer. This is why analysts increasingly view pain points as direct risk factors for both public health and financial sustainability. Addressing them is no longer optional but strategic.
Financial Pressure
The financial dimension is often the first obstacle. Digital health services promise efficiency, yet patients continue to face unexpected charges. In a CDC review more than 20% of adults in 2024 reported delaying care because of cost. That figure includes both in-person and digital services. In telehealth the problem is compounded by unclear subscription models and add-on fees for extended consultations or prescription renewals. Patients may sign up for a low advertised price but later receive bills that exceed expectations. This erodes trust quickly. Transparency in billing is now recognized as a patient safety issue, because financial stress itself worsens outcomes, especially in chronic illness management.
Time Delays
Speed was one of the promises of digital health. Patients expected that video visits would reduce waiting and triage delays. In reality many systems still operate with bottlenecks. Nearly 38% of patients in recent surveys report long digital queues before reaching a provider. The frustration is amplified because digital tools raise expectations of instant access. A rural study estimated that deferred digital consultations contributed to $8.3 billion in avoidable spending in a single year. That spending came from emergency visits and complications that could have been prevented with timely intervention. Long delays discourage patients from using digital care again and may push them back to overcrowded emergency rooms.

Technical and Usability Failures
Technical design problems are another recurring pain point. One large analysis found that only 52% of digital therapeutic apps included clear instructions or intuitive navigation. Many relied on complex language or dense menus. Poor design reduces engagement even when clinical evidence supports the tool. High digital literacy requirements effectively exclude older adults, people with cognitive impairments, and individuals for whom English is not the first language. Usability failures therefore do more than limit adoption; they deepen inequities. Developers often underestimate the need for iterative testing with diverse populations. Without it, even well-funded apps fail to achieve scale.
Security and Trust
Health data is uniquely sensitive. A breach does not only mean reputational damage but can expose details of conditions that carry stigma. Deloitte surveys show that only 35% of patients trust companies to protect their information. In independent audits less than 10% of digital therapeutic applications disclosed clear cybersecurity features. This gap is dangerous because trust once broken is hard to rebuild. Patients who doubt that their data is safe may withhold important information or avoid digital services altogether. Trust also extends to algorithmic transparency. If patients cannot understand how AI tools make recommendations, skepticism grows. Addressing this requires both technical safeguards and clear communication.
Accessibility Gaps
Digital health is often celebrated for increasing reach, but accessibility gaps remain severe. Globally about 3.8 billion people are still offline. In the United States 19 million lack reliable broadband coverage. That means digital care is inaccessible to large groups, especially in rural and underserved areas. Accessibility also concerns inclusivity for people with disabilities. Many platforms are not compatible with screen readers or lack captioning for video consultations. Patients with vision or hearing impairments are frequently excluded from digital services that should be universal. Improving accessibility is therefore not a marginal task but a central requirement for equity.
Trust and Communication
Trust in digital health is influenced not only by outcomes but by how systems communicate. Public opinion is shifting rapidly. In 2024 about 77% of UK consumers said they wanted clear disclosure when AI was used in healthcare. By 2025 that number dropped to 37% . This suggests that acceptance of AI support is rising, yet it also reflects a paradox. People may no longer insist on explicit labels, but they still expect empathy, clarity, and accountability. If communication feels robotic or dismissive, trust declines regardless of disclosure. The challenge for health providers is to integrate advanced tools while preserving a sense of human care.
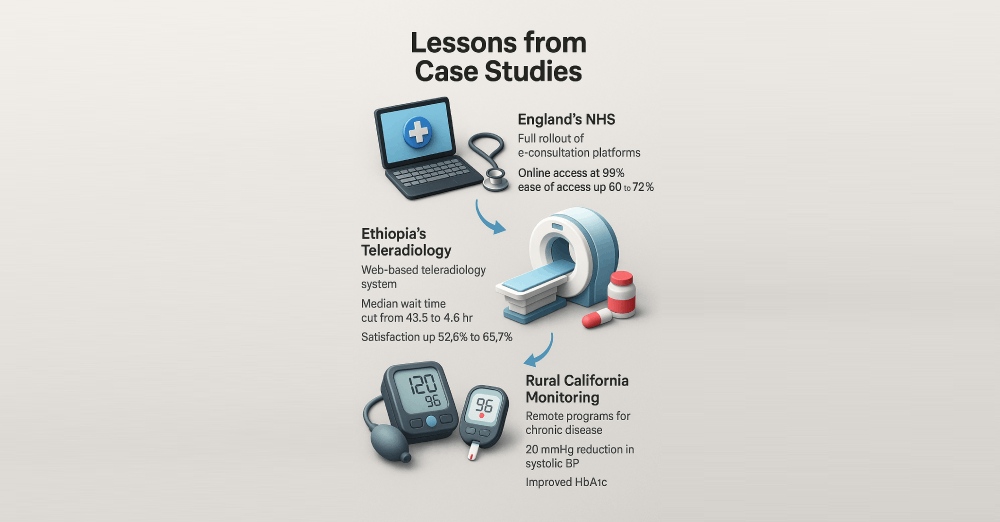
Lessons from Case Studies
- England’s NHS. After the full rollout of e-consultation platforms 99% of GP practices in England now provide online access. Patients reported a rise in ease of access from 60% in 2024 to 72% in 2025. This demonstrates that consistent digital integration across primary care can measurably improve patient satisfaction.
- Ethiopia’s Teleradiology. A web-based teleradiology system reduced the median imaging wait time from 43.5 hours to 4.6 hours. Patient satisfaction rose from 52.6% to 65.7%. This highlights how targeted digital interventions can shorten bottlenecks even in resource-limited settings.
- Rural California Monitoring. Remote monitoring programs for hypertension lowered average systolic blood pressure by 20 mmHg. Diabetic patients also achieved significant improvements in HbA1c. These results underscore that chronic disease outcomes improve when digital devices are paired with consistent coaching and clinician oversight.
Trends and Forecasts
Personalization
AI powered personalization is expanding quickly. By 2027 over 70% of providers expect to integrate predictive analytics into patient communication, moving beyond generic reminders toward tailored health nudges.
Hybrid Models
Telehealth usage increased 38 fold compared to pre-pandemic levels. Analysts forecast that hybrid care will stabilize at around 25% of visits by 2030, balancing virtual convenience with in-person necessity.
Remote Monitoring
The global remote monitoring market is projected to surpass $175 billion by 2030. The strongest growth is expected in chronic care, particularly cardiovascular disease, diabetes, and COPD.
Equity Focus
Closing digital access gaps remains a global priority. The WHO estimates that connecting 3.8 billion people who remain offline could save millions of lives by enabling access to remote consultations, vaccine information, and emergency alerts.

Regulatory Dimension
Policy frameworks are adapting quickly. The FDA cleared over 100 digital therapeutics in 2024 alone, showing rapid expansion of the category. In Europe, regulators are enforcing stricter General Data Protection Regulation (GDPR) rules on health data. In the U.S., policymakers are discussing national standards for AI disclosure in clinical contexts. These changes mean regulation is no longer a background detail but a primary driver of patient trust and company accountability.
Investment Flows
Funding patterns are shifting toward maturity. Global digital health investment reached $25 billion in 2024. Unlike the rapid but uneven growth of 2021, current capital flows prioritize proven business models such as remote monitoring and chronic care management. Investors are demanding clear evidence of outcomes and sustainable user engagement before committing to new ventures.
Role of Clinicians
Technology cannot replace clinician empathy. Surveys show that 78% of patients rank physician compassion and attentiveness as the key factors in whether they adopt digital health services. This means that training clinicians to integrate digital tools while preserving human connection is critical. Programs that blend technical onboarding with communication training are proving most effective.
Tools and Solutions
Automation through conversational AI is transforming patient interaction. In customer service outside healthcare, studies show that AI chatbots can cut wait times by more than 30%. Health systems are beginning to deploy similar models, and early evidence suggests comparable gains. The Graphlogic Generative AI & Conversational Platform enables providers to handle thousands of simultaneous patient requests while keeping responses natural and empathetic. This reduces delays, supports triage, and improves first-response resolution rates, which are key drivers of patient trust.
Accessibility is another critical frontier. Worldwide, millions of patients struggle with low health literacy or visual impairment. For these groups, traditional text-heavy apps can be barriers rather than tools. Speech interfaces are proving effective at bridging that gap. The Graphlogic Text-to-Speech API delivers prescriptions, appointment reminders, and care instructions as clear spoken language. This improves comprehension and reduces medication errors. For older adults managing multiple chronic conditions, auditory guidance can be the deciding factor in treatment adherence.
Integration of speech and conversational AI also opens opportunities for inclusivity. For instance, multilingual voice support helps non-native speakers access accurate medical instructions without relying on translations from family members. Combining these tools with robust electronic health record systems can create seamless, personalized digital care journeys.
Experts argue that the next frontier is proactive engagement: not just responding to patient queries but predicting when support will be needed and delivering it before a problem escalates. AI-driven platforms, coupled with secure data handling, can notify patients about preventive screenings or lifestyle adjustments at the right moment. This shifts healthcare from reactive problem-solving to preventive support, where every interaction becomes a step toward better outcomes.

Final Thoughts
Digital health pain points are not marginal concerns. They shape adoption rates, determine levels of trust, and directly affect outcomes. Studies indicate that when digital barriers are reduced, patient satisfaction can improve by 15% or more. At the same time, clear cost transparency has been shown to decrease care deferral by nearly 20%. These figures confirm that addressing pain points is not a branding exercise but a measurable driver of public health and financial sustainability.
Solutions must cover more than one dimension. Transparency in pricing reduces stress and delays in care. Usability upgrades make platforms intuitive for patients of all ages. Accessibility ensures that the 19 million Americans without reliable broadband, and the 3.8 billion people offline globally, are not excluded from essential services. Trust demands strict cybersecurity safeguards, as fewer than 10% of digital therapeutic apps currently disclose their protections.
Technology can be a powerful ally when guided by empathy and evidence. The Graphlogic Generative AI & Conversational Platform demonstrates how conversational AI can reduce wait times while preserving a human tone. The Graphlogic Text-to-Speech API shows how inclusivity can be embedded directly into product design, giving patients with low literacy or vision impairment real-time spoken guidance.
Ultimately, the future of digital health depends on balance. AI and automation bring efficiency, but empathy and design keep care human. When systems integrate both, they convert friction into trust and transform obstacles into measurable gains for patients, providers, and society.
FAQ
Telehealth accounts for 19% of U.S. primary care visits. Usage is expected to stabilize near 25% by 2030.
Avoidable spending from deferred digital care was estimated at $8.3 billion in one year.
Only 35% of patients feel confident about company use of health data. Cybersecurity and transparency are the biggest gaps.
Yes. In rural California remote monitoring lowered systolic pressure by 20 mmHg and improved diabetes control.

