Customer service skills are often discussed in business, but in healthcare and digital health they carry greater weight. They shape safety, trust, and loyalty. A poorly handled call or unclear email can cause frustration and also real medical risk. In business the stakes are financial, in healthcare they are personal and urgent.
Research shows that 86% of consumers stop engaging with a brand after only two negative experiences — Forbes. If the same holds in healthcare, losing a patient after two bad encounters threatens not only revenue but continuity of care. Customer service is no longer a soft skill, it is part of public health.
This article reviews the fundamentals of service skills, the role of empathy, problem solving, and technology. It also explores training, trends, and practical advice, along with a FAQ that addresses common questions in modern service delivery.

The Fundamentals of Customer Service Skills
Customer service skills include the ability to listen actively, communicate clearly, and resolve issues quickly. These skills are not abstract. They shape whether patients follow medical advice, whether clients renew contracts, and whether communities trust organizations.
The Agency for Healthcare Research and Quality has documented that communication breakdowns are among the most common causes of patient harm. A missing explanation or a misunderstood instruction can result in medication errors or missed appointments. Mastering customer service skills reduces these risks.
The World Health Organization emphasizes that patient safety depends heavily on respectful and clear interaction. This applies equally to doctors, nurses, and non clinical staff.
The core skills include:
- Active listening and empathy to understand both practical needs and emotions.
- Clear communication to avoid confusion.
- Problem solving to resolve concerns quickly.
- Adaptability to respond to diverse personalities and unexpected events.
These are not optional skills. They are as fundamental as technical knowledge.

Communication as the Foundation of Trust
Effective communication is the cornerstone of strong service relationships. It is the first signal of professionalism and care. In healthcare, this can begin with how a receptionist answers a call or how a nurse explains test results. A respectful greeting sets the tone, and every explanation that follows either strengthens or weakens trust.
When a process is explained clearly, confusion decreases and the number of repeated calls falls significantly. When communication is vague, patients may doubt the quality of care. In digital health, unclear instructions for an app or portal can discourage patients from using tools meant to support their wellbeing.
Technology now plays an important role in communication. Conversational AI platforms, such as the Graphlogic Generative AI & Conversational Platform, help professionals manage heavy workloads without sacrificing clarity. These systems analyze conversations in real time and suggest responses that maintain consistency. They cannot replace empathy, but they allow human staff to focus their attention on more sensitive cases.
The Centers for Disease Control and Prevention emphasize that health literacy depends on simple language. This principle applies beyond healthcare. Explaining terms in plain words, avoiding acronyms, and confirming comprehension are essential across industries. Asking patients or customers to paraphrase instructions is a proven technique for reducing errors.
Practical habits for effective communication include using short sentences, maintaining a positive tone, and confirming understanding before moving forward. When practiced consistently, these habits create a culture of safety and trust.

Empathy and Active Listening as Trust Builders
Empathy is not just a personal virtue, it is an evidence based skill. Research in clinical settings shows that empathetic communication improves outcomes, raises adherence to treatment, and lowers the risk of malpractice, claims National Library of Medicine. Patients who believe their concerns are taken seriously are more likely to follow advice and return for care.
Active listening supports empathy by showing attention and respect. It requires focusing fully on the person speaking, reflecting their words back, and validating their emotions. This is more than polite behavior. It reduces conflict and helps uncover the true issue behind a complaint. For example, a patient who is angry about a delayed test may actually be anxious about what the result could reveal. Recognizing that fear changes the conversation.
The measurable benefits are clear. Organizations that train empathy and listening report satisfaction scores rising by as much as 20%. They also see fewer complaints and reduced stress among staff, since conflicts are resolved earlier and with less escalation.
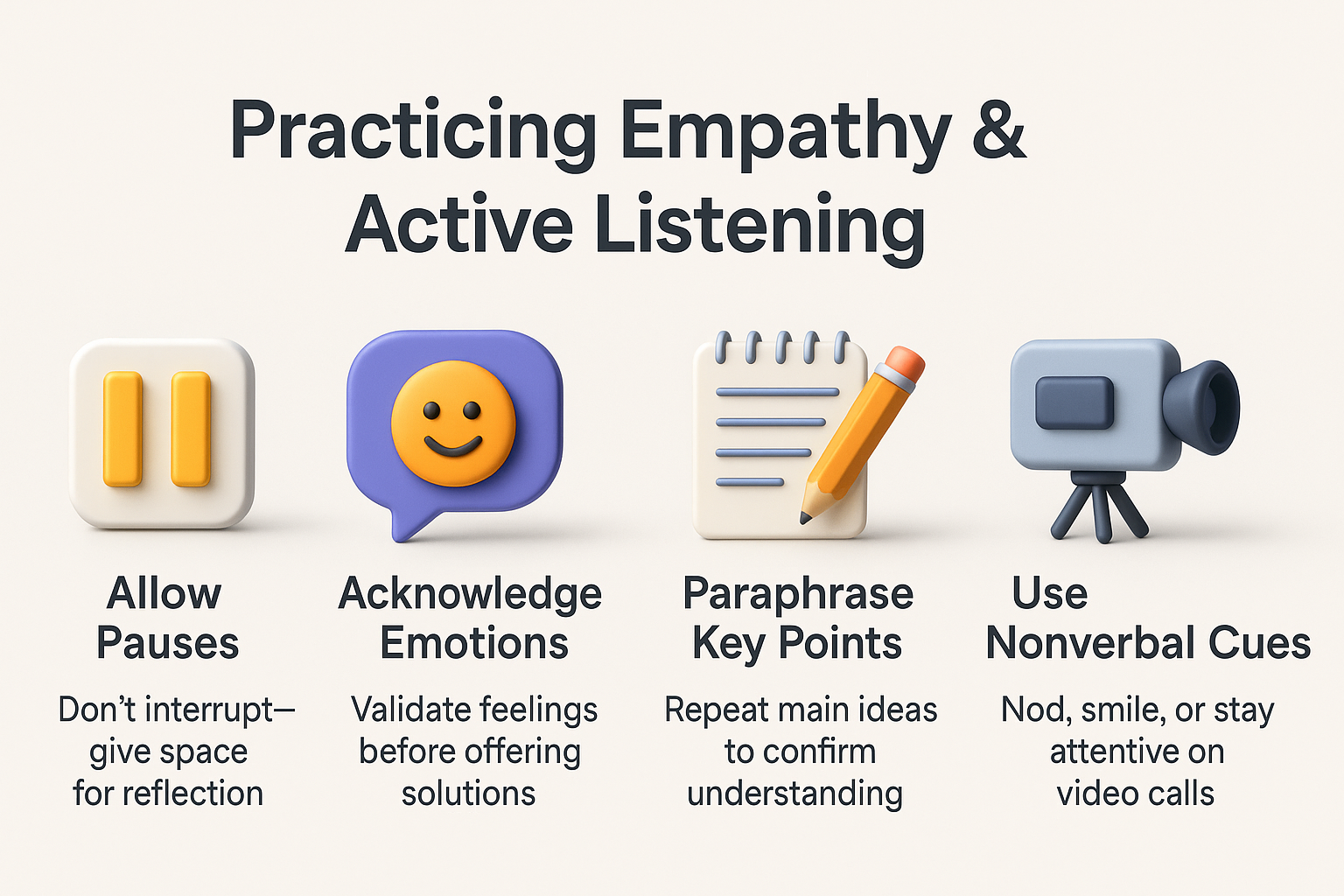
To practice empathy and active listening effectively, professionals should:
- Allow pauses without interrupting.
- Acknowledge emotions before moving to solutions.
- Paraphrase key points to confirm accuracy.
- Use nonverbal cues such as nodding or maintaining attention in video calls.
These practices turn routine interactions into moments of connection, strengthening loyalty and reducing long term risk.
Adaptability and Problem Solving
No two service interactions are the same. A family calling about a billing error requires a different tone than a patient worried about symptoms. Adaptability allows staff to adjust communication style to each situation without losing professionalism.
Problem solving is equally essential. It involves breaking complex issues into manageable steps, maintaining composure, and guiding the person through each stage. A patient struggling with an online health portal may need a calm, step by step explanation with pauses to confirm understanding. This prevents frustration and increases confidence in the service.
Industry data indicates that teams who train both adaptability and structured problem solving see satisfaction rise by around 20%. This gain demonstrates that flexibility and structure are not conflicting qualities. They work best together. Flexibility ensures that communication feels personal. Structure ensures that issues are resolved consistently and effectively.
To cultivate adaptability and problem solving, organizations can:
- Encourage staff to practice different communication tones through role playing.
- Teach structured problem solving frameworks that break down issues systematically.
- Provide stress management training to help staff stay calm under pressure.
- Offer feedback sessions that highlight both successes and missed opportunities.
Adaptable problem solvers can de-escalate conflicts, protect trust, and build resilience. These qualities are critical in healthcare, where lives can be impacted by the quality of a single conversation.

Technology as Amplifier not Replacement
Digital fluency is now expected of every service professional. Customer relationship management systems, scheduling platforms, and automated speech tools reduce waiting times and allow smoother coordination. A well trained agent can retrieve a patient’s medical record or a customer’s history within seconds. That speed shortens calls, lowers stress, and builds trust.
Automation provides efficiency, but it cannot replace the human element. Over reliance on chatbots can frustrate people who want compassion. For example, a patient asking about test results may not want a scripted answer. They want reassurance, context, and emotional recognition.
The Graphlogic Text-to-Speech API shows how technology can complement staff. It transforms written instructions into natural speech, which helps agents deliver information faster while still keeping a personal voice. This balance demonstrates how digital tools can extend human capacity without erasing empathy.
The National Institutes of Health stresses that technology should support clinical judgment rather than replace it. The hybrid model has emerged as the most effective solution. In this model, AI handles routine questions and frees staff to focus on complex or emotional cases. This approach reduces burnout while ensuring patients receive both speed and empathy.

Professionalism and Proactive Support
Professionalism is more than good manners. It is patience, respect, and adherence to ethical standards in every interaction. A professional response during tense moments can calm an upset patient or reassure a frustrated customer. This behavior reflects positively on the organization as a whole.
Proactive support takes professionalism a step further. Instead of waiting for issues to escalate, organizations act early. For example, if a hospital notices frequent questions about discharge instructions, creating a detailed FAQ can reduce repeated calls. Patients leave with clearer guidance, and staff save time.
When professionalism and proactive service are combined, organizations consistently see higher retention and more referrals. Patients and clients begin to see the provider as both reliable and caring. This reputation is built slowly but can be lost quickly if standards slip.
Continuous Learning and Development
Skills do not remain sharp without practice. Continuous learning is therefore essential. It ensures that staff keep pace with evolving standards, technologies, and patient needs.
Options for ongoing development include structured workshops, self paced online courses, peer feedback sessions, and self assessment exercises. Among these, role playing often produces the fastest gains. Practicing difficult conversations in a controlled environment helps staff prepare for real world challenges.
Teams that engage in regular training sessions often report satisfaction metrics rising by up to 20% within a single quarter. This is not only about customers. Evidence published in BMJ Open Quality shows that continuous training improves patient outcomes and strengthens staff morale. It reduces errors, improves adaptability, and sustains motivation in high stress environments.
Continuous development also builds resilience. Staff who train consistently are better able to adjust to new technologies, changing policies, and unexpected scenarios. This flexibility is increasingly valuable in both healthcare and digital service sectors.
Trends and Forecasts in Customer Service
- Customer service is shifting from reactive to predictive. AI tools can now analyze patterns in calls and emails to anticipate common problems before they escalate. In healthcare, this might mean identifying recurring concerns about side effects or billing cycles and addressing them in advance.
- Another strong trend is multimodal communication. Patients and clients expect to move between phone, chat, video, and email without repeating their information. This seamless integration requires coordination between systems and training for staff. Virtual assistants powered by natural language processing are becoming standard in this environment.
- By 2030, industry analysts forecast that more than 70% of service interactions will include some form of AI support. At the same time, surveys show that over 60% of customers still prefer human contact when dealing with sensitive issues. This means the hybrid model, where AI handles routine questions and humans focus on complex or emotional matters, will dominate.
- Ethical transparency is also a rising priority. Customers and patients want to know if they are communicating with AI or with a human. Regulators may soon make disclosure mandatory. Organizations that adopt transparency early will build trust and reduce backlash.

Practical Tips for Professionals
Improving service quality does not always require large investments or complex systems. Often the most effective strategies are simple habits that staff can apply daily. These practices reduce errors, improve safety, and create stronger relationships with patients and customers.
- Confirm understanding. Ask the customer or patient to repeat instructions in their own words. This ensures that the message has been received clearly and highlights any points of confusion immediately. In healthcare, this method is known as the “teach back” technique and is widely recommended for improving adherence to treatment.
- Use plain language. Avoid jargon, acronyms, and technical terms unless they are explained. Simple words are easier to process under stress, especially in medical contexts. For example, saying “high blood pressure” instead of “hypertension” makes information more accessible to patients with varying levels of health literacy.
- Take clear notes. Document each interaction thoroughly. This helps maintain continuity when customers switch channels, such as moving from phone support to live chat. Accurate notes also reduce repetition and frustration, since the customer does not need to explain the same issue multiple times.
- Anticipate recurring issues. Prepare ready made explanations and resources for common concerns. For example, if many patients call about billing cycles, a clear FAQ or automated response can save staff time and reduce waiting. This proactive approach signals that the organization values efficiency and respect for the customer’s time.
- Balance speed with empathy. Efficiency is important, but rushing can make interactions feel cold. Allow space for emotional responses. A brief pause to acknowledge frustration or anxiety often makes customers more receptive to solutions. Even short empathetic statements, such as “I understand this has been stressful,” can transform the tone of the conversation.
When applied consistently, these five practices create a strong service culture. They lower the risk of miscommunication, reduce safety incidents, and build long term loyalty. For professionals in healthcare and digital service industries, they represent small changes with significant impact.
Conclusion
Customer service is no longer a secondary function. In healthcare and technology it is a primary driver of trust, safety, and loyalty. Clear communication, empathy, adaptability, and problem solving are not optional. They are core competencies.
Technology, including advanced platforms and APIs, strengthens these skills when used wisely. Yet the human connection must remain at the center. Organizations that embrace continuous learning and balance digital efficiency with empathy will see measurable gains in satisfaction and loyalty.
The future belongs to those who understand that service is not only about solving problems but also about building relationships that last.
FAQ
Because they influence patient safety, adherence to treatment, and overall trust. Poor service can result in missed medication, incorrect follow up, or loss of continuity of care.
Empathy validates emotions and makes patients feel understood. Research shows empathetic encounters improve adherence and reduce malpractice risk.
No. Technology is an amplifier. AI and speech tools handle routine tasks, but humans remain essential for sensitive, complex, and emotional cases.
Through continuous training, role playing, feedback, and self assessment. Online courses and peer reviews also help maintain sharp skills.
Interrupting customers, ignoring emotions, over relying on scripts, and failing to follow up. Each of these mistakes erodes trust and satisfaction.

